How to step over the learning curve of laparoscopic spleen-preserving splenic hilar lymphadenectomy
Introduction
As the reported incidence of No. 10 lymph node metastases is about 9.8–20.9% (1), the lymph nodes in the splenic hilar area should be dissected for D2 LN dissection during total gastrectomy for advanced proximal gastric cancer (2). Spleen-preserving splenic hilar lymphadenectomy is now widely used in total gastrectomy with D2 LN dissection since its first introduce in 2008 (3), due to the significantly increased postoperative morbidity and mortality after splenectomy (4-6). Meanwhile, with the rapid development of minimally invasive surgery, the laparoscopy-assisted gastrectomy for gastric cancer is gradually accepted. However, due to vessel variation, complicated anatomy and deep location of splenic hilum, as well as the difficulty to manage splenic or vascular bleeding at the splenic hilum, the procedure of laparoscopic spleen-preserving No. 10 lymph node dissection remains a challenge for gastric surgeons. Recently, professor Huang and his colleagues have introduced “Huang’s three-step maneuver” for laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer (7). It does make the procedure easier. But it seems that skilled surgeon and well-coordinated team are needed for the performance. With the aim to help unskilled surgeons to step over the learning curve for laparoscopic spleen-preserving No. 10 lymph node dissection, here we introduce our experiences in the procedure.
Patient selection and workup
Patients for this operation should be diagnosed as proximal gastric cancer, which have a pre-operative stage of cT2-3NxM0, with gastroscopic biopsy and contrast computed tomography, including cancers of the esophagogastric junction (EGJ, Siewert type III).
Inclusion criteria: (I) proximal gastric adenocarcinoma (including Siewert type III EGJ cancer) with biopsy; (II) pre-operative stage of cT2-3NxM0 with contrast computed tomography; (III) age from 20 to 70 years old.
Exclusion criteria: (I) T1 orT4 tumor; (II) distal metastasis detected before or during operation; (III) apparent lymph nodes fusion; (IV) history of previous gastrectomy; (V) pre-operative neoadjuvant chemotherapy or radiotherapy; (VI) age beyond 70 years old; (VII) with severe systemic problems that can’t endure major operations.
Pre-operative preparation
- Careful pre-operative examinations to exclude any contraindication;
- Proactive preparation of respiratory system for 3 days;
- Proactive mental preparation of the patients before operation;
- Inserting gastric tube and urethral catheter right before operation;
- Preparation of all instruments needed for the operation.
Equipment preference card
- Laparoscopy system, including a high-definition camera, display system, and pneumoperitoneum machine;
- Irrigation and suction devices;
- Image and video storage devices;
- Ultracision;
- Bioactive coagulation set;
- Intestinal Endo-GIA;
- Circular staplers;
- 5–12 mm trocars;
- Intestinal forceps;
- Maryland forceps;
- Noninvasive grasping forceps;
- Scissors;
- Needle holder;
- Absorbable suture;
- Aspirator;
- Absorbable clip applier;
- Titanium clip applier;
- Vascular clamps;
- Small gauzes.
Procedure
Patient’s position
Patient position is very important for intraoperative exposure during laparoscopic gastrectomy. A reverse Trendelenburg position with the head elevated up approximately 15 degrees and tilted left side up at approximately 25 degrees is used. This position allows the intestine and omentum to move toward the lower right abdominal cavity and it will help to expose the splenic hilar area.
Trocar locations
As the trocars’ position, here we make a little change. In routine procedure, the 5-port method (8) is generally used. We lower the observation port to 2–3 cm below the umbilicus. We also move the major hand port (with the surgeon on the patient’s right side) closer to the splenic hilar area, which is located in the middle of the observation port and the tractive one, to overcome the shortness of the ultracision during splenic hilar lymphadenectomy.
Surgeons’ locations
During the most part of the operation, the surgeon stands on the patient’s left side with the assistant on the right and the camera operator between the patient’s legs. But the surgeon and the assistant change their locations when it comes to the splenic hilar lymphadenectomy without any change of the camera operator.
Operation procedure
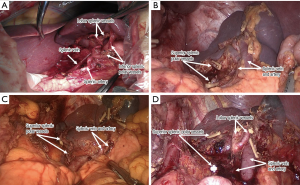
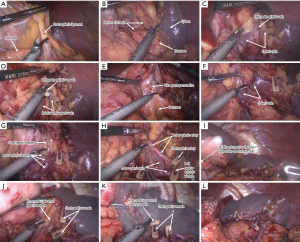
Routine procedure (Figure 1): in patients with normal BMI and without much difficulty for splenic hilum exposure, we follow routine procedure.

Step 1. Exposure of the cauda pancreatis and dissection of No. 4sb lymph nodes and lymph nodes around the inferior lobar splenic vessels. The assistant puts the omentum on the anterior wall of the stomach. His or her right hand pulls up the gastrosplenic ligament and gastrocolic ligament at the point close to the stomach, and pulls down and caudalward the transverse and splenic flexure of colon with his or her left hand, then the surgeon divides the gastrocolic ligament along the transverse colon to expose the cauda pancreatis and the inferior pole of the spleen, then peels the anterior pancreatic fascia of the pancreatic cauda from the inferior margin of the pancreas up to the superior margin and enters the upper retropancreatic space. At this time the inferior lobar splenic vessels will usually be exposed. Then the surgeon can continue to dissect the vessels towards the splenic hilum until they enter the spleen. The left gastroepiploic vessels usually derive from the inferior lobar splenic vessels and can be seen then. The assistant’s right hand pulls up the lymphatic fatty tissue on the surface of the vessels gently at the point close to the stomach, and his or her left hand pulls down and caudalward the splenic flexure of colon or the cauda pancreatis. Then the surgeon meticulously dissects the vessels to their roots and divides them at the roots.
Step 2. Exposure of the trunk of splenic vessels and dissection of No. 11d lymph nodes. The assistant’s right hand moves to the upper gastric body at the greater curvature side, and his or her left hand pulls down and caudalward the mesentery of transverse colon at the root. Then the surgeon can peel the fascia of pancreatic body from the inferior margin of the pancreas up to the superior margin and enter the upper retropancreatic space to expose the trunk of splenic vessels and then continue to dissect No. 11d lymph nodes. After entering the upper retropancreatic space, the assistant’s left hand will press down and caudalward the pancreatic body with small gauze. To be convenient, we suggest opening the sheath of the splenic vein trunk during lymphadenectomy. The surgeon’s left hand can lift up the fatty lymphatic tissue around the trunk of splenic vessels and his or her right hand can dissect along the splenic vessels with ultracision towards splenic hilum until the crotch of the inferior and superior lobar splenic vessels appears. The inferior lobar splenic vessels have already been revealed during the dissection of No. 4sb lymph nodes.
Step 3. Dissection of No. 10 lymph nodes and management of the upper pole of the spleen. The assistant’s right hand then pulls up the gastrosplenic ligament gently at the point close to the stomach, and his or her left hand presses down and caudalward the cauda pancreatis with small gauze. And the surgeon dissects along the superior lobar splenic vessels carefully and gently. During the dissection, we will encounter several short gastric vessels, which are derived from the superior lobar splenic vessels. The surgeon should denude them and divide them at their roots.
The uppermost short gastric vessel is usually the shortest one and is easily to be injured. Thus, when the surgeon dissects close to the upper pole of the spleen, the assistant’s left hand should pull the stomach to the lower right of the abdominal cavity to attain well exposure. And then the surgeon can dissect and denude the uppermost short gastric vessel meticulously and divide it at its root. Then the laparoscopic spleen-preserving splenic hilar lymphadenectomy can be completed successfully.
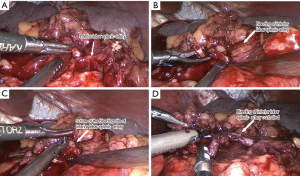
Modified procedure (Figure 2): in patients with high BMI or bulky stomach that causes difficulties for splenic hilum exposure, we suggest modified procedure.

Step 1. In this step, the procedure is the same with step1. In routine procedure.
Step 2. Division of the gastrosplenic ligament in advance and exposure of the trunk of splenic vessels and dissection of No. 11d lymph nodes. When we are in trouble for splenic hilar lymphadenectomy, especially in patients with high BMI or bulky stomach, the exposure of the splenic hilum will be difficult, we can consider dividing the gastrosplenic ligament after we finish step 1 procedure. After exposure of the cauda pancreatis and dissection of No. 4sb lymph nodes, the assistant’s right hand grasps the stomach at the greater curvature side, and his or her left hand pulls down and caudalward the splenic flexure of colon. Then the surgeon can easily divide the gastrosplenic ligament along the greater curvature of the stomach and dissect the No. 2 lymph node passingly to expose the left side of the cardia with ultracision. And then exposure of the trunk of splenic vessels and dissection of No. 11d lymph nodes can be continued as described in step 2 of routine procedure.
Step 3. Dissection of No. 10 lymph nodes and management of the upper pole of the spleen. The assistant can put the stomach lower right of the abdominal cavity to gain a well visual field of the splenic hilum and his or her right hand can be freed to assist the surgeon to finish the dissection of No. 10 lymph nodes and to manage the upper pole of the spleen, and even when the bleeding of the splenic vessels occurs, the assistant’s right hand can help the surgeon to manage the situation well to avoid conversion to open surgery. The assistant’s right hand pulls up the divided gastrosplenic ligament, and his or her left hand presses down and caudalward the cauda pancreatis with small gauze. The surgeon dissects along the superior lobar splenic vessels carefully and gently and denudes all the short gastric vessels, which are derived from the superior lobar splenic vessels and divides them at their roots to finish the lymphadenectomy.
Role of team members
- Surgeon: perform the major part of the operation;
- Assistant: help to expose the visual fields of the operation and assist the surgeon to perform the operation successfully;
- Camera operator: in charge of the camera system to gain a sharp and comfortable view of the operation;
- Anesthetist: in charge of the patient’s anesthesia to make sure the patient is under well anesthetic state during the operation;
- Nurses: in charge of the devices needed for the operation before and during operation.
Post-operative management
- Parenteral nutrition for 5–7 days after operation;
- Out-of-bed activity on day 2;
- Extract gastric tube after passage of gas by anus;
- Liquid diet the next day after extraction of gastric tube;
- Semi-liquid diet on day 7 and extract peritoneal cavity drainage tubes;
- Discharge on day 8.
Tips, tricks and pitfalls
Due to vessel variation, complicated anatomy and deep location of splenic hilum, laparoscopic splenic hilar lymphadenectomy has become one of the difficulties of laparoscopic radical gastrectomy for gastric cancer. How to step over the learning curve of laparoscopic splenic hilar lymphadenectomy becomes a challenge for gastric surgeon. For two years’ clinical practices, we have already successfully performed 56 cases of laparoscopic spleen-preserving splenic hilar lymphadenectomy, 49 ones with 2D laparoscopy and 7 ones with 3D laparoscopy respectively, without any severe complications and conversion to open surgery. But three cases of bleeding of lobar splenic vessels occurred and five cases of partly spleen ischemia (which was considered as the ischemia range reached almost 1/4 of the spleen, but focal spleen ischemia was not included in that) were found after splenic hilar lymphadenectomy. No infarction of spleen occurred in all these cases. The followings are our experiences for stepping over the learning curve of laparoscopic splenic hilar lymphadenectomy.
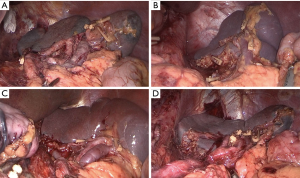
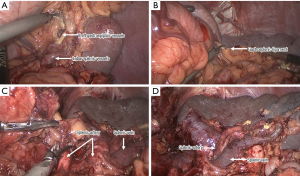
Firstly, the surgeons should be familiar with the anatomy of splenic hilum. The splenic vessels go along the pancreas in the retropancreatic space at the superior border of the corpus and cauda pancreatis, and give off lobar splenic vessels when they are close to the splenic hilum. The two-branch type possesses highest ratio (11-13) [in our data, it takes 83.99% (47/56)], but the one-branch (5.36%, 3/56), three-branch (7.14%, 4/56), or multiple-branch (3.57%, 2/56) is infrequent (Figure 3). The two-branch one is typical type of splenic hilar vessels. The inferior lobar branch is usually short and thick. The left gastroepiploic vessels and one to two lower short gastric vessels are usually derived from the inferior lobar splenic vessels. And the superior lobar branch is usually long and thin. This branch does not enter the spleen immediately but go upwards along the surface of the spleen and gives off short gastric vessels and then enters the superior pole of the spleen. The uppermost short gastric vessel is always the shortest one so that it’s easily to be injured. In addition, in several patients, there’s splenic polar vessel (Figure 4). It’s vessel that does not pass by the splenic hilum but enter the spleen directly. The inferior polar splenic vessel is usually short and thick and close to the spleen, it won’t increase the difficulties for splenic hilar lymphadenectomy. The superior polar splenic vessel is usually long and thin and distal to the splenic hilum, and is not easily to be distinguished from posterior gastric vessels. We do find that in several patients, the superior polar splenic vessels are too thin that it does not affect the blood supply of the spleen even when they are cut off. So when we find a thin superior polar splenic vessel during the lymphadenectomy, we can try to clamp the vessel to observe the color of the spleen. If the color does not change, then we can cut off the vessel directly so as to simplify the procedure.
Secondly, we can divide the gastrosplenic ligament in advance if it’s necessary (Figure 5). When we are in trouble with splenic hilar lymphadenectomy, especially in overweight patients or patients with bulky stomach and the exposure of the splenic hilum is difficult, we can consider dividing the gastrosplenic ligament in advance. Due to the relative easiness for No. 4sb lymph node dissection, we usually dissect the No. 4sb lymph node firstly and then divide the gastrosplenic ligament, and dissect the No. 2 lymph node to expose the left side of the cardia. Then we can put the stomach in the lower right of the abdominal cavity and continue the splenic hilar lymphadenectomy. In this step, the assistant’s right hand can be freed from exposure of the hilum to assist the surgeon to perform the lymphadenectomy. Even when the vessel injury occurs, it would be easier to control the bleeding and avoid conversion to open surgery (Figure 6).
But there are two disadvantages for this method. The first one is that en-block dissection cannot be achieved. The second one is that the favorable tension provided by the assistant’s pulling up the gastrosplenic ligament will be lost. Therefore, we prefer to consider this method as a tool for stepping over the learning curve of laparoscopic splenic hilar lymphadenectomy.
Thirdly, we can change the surgeon and the assistant’s position. In classical laparoscopic splenic hilar lymphadenectomy, the surgeon usually stands between the patient’s legs, and both the assistant and the camera operator stand rightward. In this kind of position, due to the narrow space, the assistant and the camera operator will interfere with each other. And the surgeon’s right and left hands present a kind of up and down relationship, it will be inconvenient for operating. Besides, the angle of the ultrasonic scalpel’s operating direction and the splenic vessels’ direction will be larger, it’ll bring inconvenience for the dissection and exposure of splenic vessels.
We take the position that the surgeon stands on the right side of the patient, with the camera operator between the patient’s legs and the assistant on the left side. In this kind of position, the surgeon, the assistant and the camera operator will not interfere with each other. And the left and right relationship of the trocars for the surgeon will provide convenience for operating. In addition, the angle of the ultrasonic scalpel’s operating direction and the splenic vessels’ direction will be smaller, it’ll bring convenience for the dissection and exposure of splenic vessels.
Fourthly, we should routinize the splenic hilar lymphadenectomy. We divide the splenic hilar lymphadenectomy into several relatively regular operating steps to make the operating procedure more rationalized and the team cooperation more unhindered, as described in the operation procedure part (Figure 7).
In conclusion, we introduce our experiences in the procedure of laparoscopic spleen-preserving splenic hilar lymphadenectomy, and with more than 50 cases’ practice we find it does can make the procedure easier. We sincerely hope that it would help unskilled surgeons to step over the learning curve of the procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Mönig SP, Collet PH, Baldus SE, et al. Splenectomy in proximal gastric cancer: frequency of lymph node metastasis to the splenic hilus. J Surg Oncol 2001;76:89-92. [Crossref] [PubMed]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113-23. [Crossref] [PubMed]
- Maruyama K, Sasako M, Kinoshita T, et al. Pancreas-preserving total gastrectomy for proximal gastric cancer. World J Surg 1995;19:532-6. [Crossref] [PubMed]
- Hyung WJ, Lim JS, Song J, et al. Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 2008;207:e6-11. [Crossref] [PubMed]
- Okabe H, Obama K, Kan T, et al. Medial approach for laparoscopic total gastrectomy with splenic lymph node dissection. J Am Coll Surg 2010;211:e1-6. [Crossref] [PubMed]
- Sakuramoto S, Kikuchi S, Futawatari N, et al. Laparoscopy-assisted pancreas- and spleen-preserving total gastrectomy for gastric cancer as compared with open total gastrectomy. Surg Endosc 2009;23:2416-23. [Crossref] [PubMed]
- Huang CM, Chen QY, Lin JX, et al. Huang's three-step maneuver for laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer. Chin J Cancer Res 2014;26:208-10. [PubMed]
- Huang CM, Zheng CH. Preoperative Notes of Laparoscopic Lymph Node Dissection for Gastric Cancer. In: Huang CM, Zheng CH, editors. Laparoscopic Gastrectomy for Gastric Cancer: Surgical Technique and Lymphadenectomy. Berlin: Springer Netherlands, 2015:13-24.
- Hong QQ, Li YW, You J, et al. Routine procedure. Asvide 2016;3:219. Available online: http://www.asvide.com/articles/977
- Hong QQ, Li YW, You J, et al. Modified procedure. Asvide 2016;3:220. Available online: http://www.asvide.com/articles/978
- Treutner KH, Klosterhalfen B, Winkeltau G, et al. Vascular Anatomy of the Spleen. Clin Anat 1993;6:1-8. [Crossref]
- Pandey SK, Bhattacharya S, Mishra RN, et al. Anatomical variations of the splenic artery and its clinical implications. Clin Anat 2004;17:497-502. [Crossref] [PubMed]
- Zheng CH, Xu M, Huang CM, et al. Anatomy and influence of the splenic artery in laparoscopic spleen-preserving splenic lymphadenectomy. World J Gastroenterol 2015;21:8389-97. [Crossref] [PubMed]
Cite this article as: Hong QQ, Li YW, Huang ZJ, Luo LT, Luo Q, You J. How to step over the learning curve of laparoscopic spleen-preserving splenic hilar lymphadenectomy. J Vis Surg 2016;2:98.